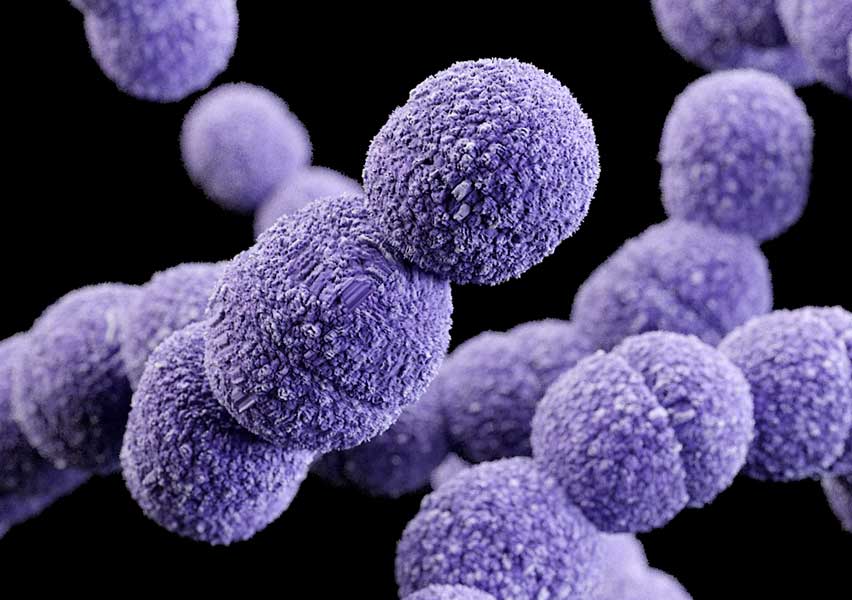
Streptococcus agalactiae
Streptococcus agalactiae, also known as Group B Streptococcus (GBS), is a gram-positive, beta-hemolytic coccus that forms chains. It is catalase-negative, facultative anaerobic, and part of the normal gastrointestinal and genitourinary flora in healthy adults. Despite its commensal nature, GBS can cause serious infections, especially in neonates, pregnant women, elderly, and immunocompromised individuals. Based on capsular polysaccharide structure, ten antigenically distinct serotypes (Ia, Ib, II–IX) have been identified.
Clinical Features
Streptococcus agalactiae is the leading cause of neonatal sepsis and meningitis in developed countries. Neonatal infections are classified as early-onset (within the first week of life) or late-onset (from 7 days to 3 months). Early-onset disease is often due to vertical transmission during delivery.
Risk factors include preterm birth, prolonged rupture of membranes (>18 hours), intrapartum fever, maternal GBS bacteriuria during pregnancy, and history of GBS disease in previous infants.
In adults, GBS can cause urinary tract infections, bacteremia, pneumonia, endocarditis, and obstetric complications such as chorioamnionitis and postpartum sepsis.
Diagnosis
Diagnosis is based on culture from blood, cerebrospinal fluid, urine, or other clinical specimens. Identification methods include:
- Beta-hemolysis on blood agar.
- Positive CAMP test.
- Hippurate hydrolysis.
- Growth with red pigmentation on Granada medium (granadaene).
- Latex agglutination for Group B antigen.
- Molecular detection via PCR or NAATs.
- MALDI-TOF mass spectrometry.
Treatment
Penicillin or ampicillin is the first-line treatment. In penicillin-allergic patients, cefazolin, vancomycin, or clindamycin may be used depending on susceptibility. For perinatal prevention, intrapartum antibiotic prophylaxis is administered to colonized pregnant women to prevent neonatal disease.