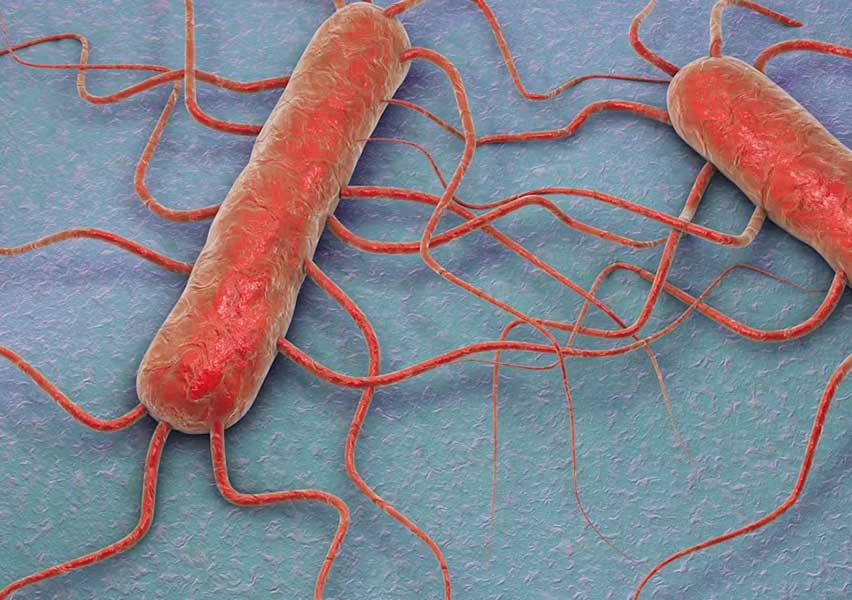
Listeria monocytogenes
Listeria monocytogenes is a facultative intracellular Gram-positive rod and one of the most virulent foodborne pathogens, with a case-fatality rate between 20% and 30%. It can grow over a wide range of temperatures (1 °C to 45 °C) and tolerate high salt concentrations, allowing survival in refrigerated or processed foods. It primarily affects immunocompromised individuals, pregnant women, newborns, and the elderly.
Clinical features:
Listeriosis may be invasive or non-invasive. Invasive listeriosis includes:
- Meningitis
- Encephalitis
- Sepsis
- Granulomatosis infantiseptica
- Miscarriages and neonatal infections
In healthy individuals, it typically manifests as a self-limited febrile gastroenteritis. During pregnancy, L. monocytogenes can cross the placenta, leading to fetal infection or death. The bacterium uses InlA and InlB surface proteins to bind to E-cadherin and Met receptors, triggering host cell invasion. Once inside, it escapes the phagosome via listeriolysin O (LLO) and phospholipases, then uses ActA to hijack the host’s actin for intracellular motility and intercellular spread, thus avoiding humoral immune responses.
Diagnosis:
Diagnosis includes:
- Blood agar culture (grayish colonies with beta-hemolysis)
- CAMP test (positive synergistic hemolysis with Staphylococcus aureus)
- Bile esculin hydrolysis (black coloration indicates positivity)
- Motility at 25 °C ("umbrella-like" pattern in semi-solid medium)
- Voges-Proskauer test (positive for fermentative metabolism)
- Molecular testing and blood/CSF cultures in systemic infections
Isolation from sterile sites like blood or CSF confirms diagnosis in invasive disease.
Treatment:
Preferred therapy includes:
- Ampicillin or penicillin G in combination with gentamicin
- For penicillin-allergic patients: trimethoprim-sulfamethoxazole
L. monocytogenes is resistant to natural penicillins, β-lactamase-resistant penicillins, and all cephalosporins. Early and prolonged antibiotic therapy (2–6 weeks or more) is crucial, especially in severe infections such as neonatal sepsis or meningoencephalitis. In immunocompromised patients, treatment may need to be extended to prevent relapses.