
Influenza A & B
What is influenza (flu)?
Influenza, commonly known as flu, is an infectious disease caused by RNA viruses that mainly affect the respiratory tract. Influenza viruses are known for their high genetic variability and are classified into types A, B and C.
Frequent mutations lead to changes in viral surface glycoproteins, which are responsible for the seasonal epidemics and occasional pandemics associated mainly with Influenza A and Influenza B viruses.
In the case of Influenza A, the ability to exchange genetic material between human and animal viruses allows the emergence of new subtypes, such as H1N1, H3N2 or H5N1, increasing the epidemiological relevance of this virus and highlighting the importance of accurate laboratory surveillance.
Clinical characteristics and transmission
In humans, influenza affects the upper and lower respiratory tract and spreads easily from person to person, especially in environments with close contact such as schools, workplaces, hospitals, and long-term care facilities.
The infection usually lasts around one week and is commonly associated with symptoms such as:
- High fever
- Muscle aches
- Headache
- Sore throat
- Cough
Although most patients recover without complications, influenza can cause severe disease in children, older adults, and individuals with underlying medical conditions, potentially leading to pneumonia, hospitalization, or even death. This makes early and accurate diagnosis essential, particularly during peak flu season.

Influenza season and current epidemiological context
During the 2025 winter season, influenza activity has increased earlier and more intensely than in previous years across several European countries. Surveillance data show Influenza A as the predominant circulating virus, with A(H3N2) and A(H1N1)pdm09 among the most frequently detected subtypes.
This epidemiological scenario underlines the need for robust diagnostic strategies that go beyond symptom-based assessment, enabling laboratories to deliver reliable results even when multiple respiratory viruses are co-circulating.
Why laboratory diagnosis is critical during flu epidemics
Outside epidemic periods, isolated influenza cases can be difficult to diagnose clinically. During epidemics, diagnosis becomes even more challenging due to the overlap of symptoms with other respiratory infections such as RSV or SARS-CoV-2.
For this reason, laboratory diagnosis plays a key role, particularly in high-risk patients and during periods of high viral circulation. While serological methods such as ELISA and immunofluorescence remain useful in certain situations, molecular techniques, especially real-time PCR, have become the reference approach due to their speed, sensitivity, and specificity.
A molecular approach to influenza diagnostics
During respiratory season, laboratories face increasing testing volumes and the co-circulation of multiple respiratory viruses with overlapping clinical symptoms. In this context, a stepwise molecular diagnostic strategy allows laboratories to combine speed, accuracy and actionable information, adapting the depth of analysis to each clinical or epidemiological need.
Vircell’s molecular workflow for influenza diagnostics is designed to support this approach, moving from broad multiplex screening to targeted Influenza A subtyping, while ensuring reliability through dedicated quality controls.
Multiplex screening of respiratory viruses
SARS-COV-2 / FLU A / FLU B / RSV REALTIME PCR KIT (RTPCR021)
- Real-time RT-PCR multiplex assay for the simultaneous detection of Influenza A, Influenza B, RSV and SARS-CoV-2 from a single respiratory sample.
- Covers the most prevalent respiratory viruses, supporting rapid differential diagnosis during periods of high viral circulation.
- Reduces hands-on time and optimizes laboratory workflows in high-demand seasonal settings.
- Fully aligned with WHO and ECDC diagnostic algorithms, which recommend initial molecular screening for respiratory viruses as the first step in influenza diagnosis.
- Allows early identification of Influenza A–positive samples, providing the basis for further confirmatory testing when required.

Influenza A subtyping for confirmation and surveillance
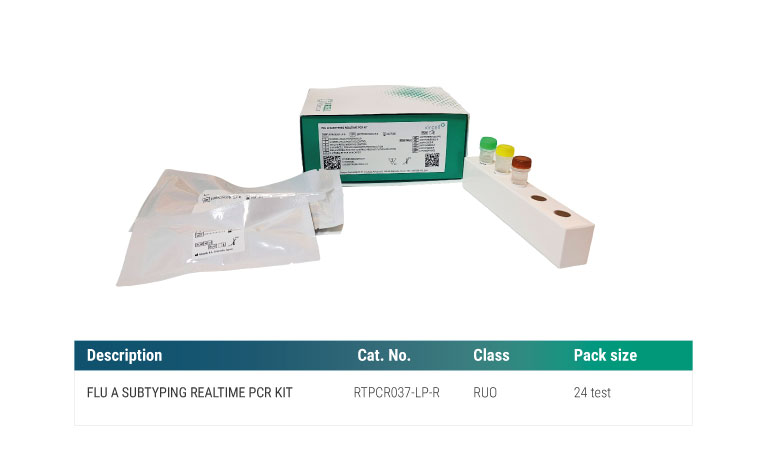
FLU A SUBTYPING REALTIME PCR KIT (RTPCR037-LP-R)
- Real-time RT-PCR assay designed to detect and differentiate epidemiologically relevant Influenza A subtypes: A(H1N1)pdm09, A(H3N2) and A(H5).
- Intended as a confirmatory assay following Influenza A detection, in line with WHO and ECDC recommendations.
- Supports subtype-level confirmation, which is essential for epidemiological surveillance, outbreak monitoring and public health response.
- In cases where avian subtypes such as H5 or H7 are detected, international guidelines recommend further genotyping, reinforcing the importance of accurate molecular subtyping.
- Provides actionable subtype information during intense or early influenza seasons, when precise characterization is critical.
A complete influenza diagnostic portfolio
Influenza diagnostics often require more than a single technique. Vircell provides a comprehensive influenza portfolio, including: Multiplex real-time PCR kits for respiratory virus screening, molecular controls for quality assurance, and serological and immunofluorescence assays for antibody detection
Together, these solutions support laboratories at every stage of influenza diagnosis, helping them respond effectively to seasonal peaks and evolving epidemiological challenges.

